Type 2 Diabetes: PART 1 – Let’s not sugarcoat it
Welcome to this two-part blog series covering everything you need to know about type 2 diabetes.
Did you know that in Australia, type 2 diabetes represents up to 90% of all diabetes cases! In fact, 1 person develops type 2 diabetes every 5 minutes. There are also up to 500,000 people in Australia who have undiagnosed type 2 diabetes.
Type 1 versus Type 2- What's the difference?
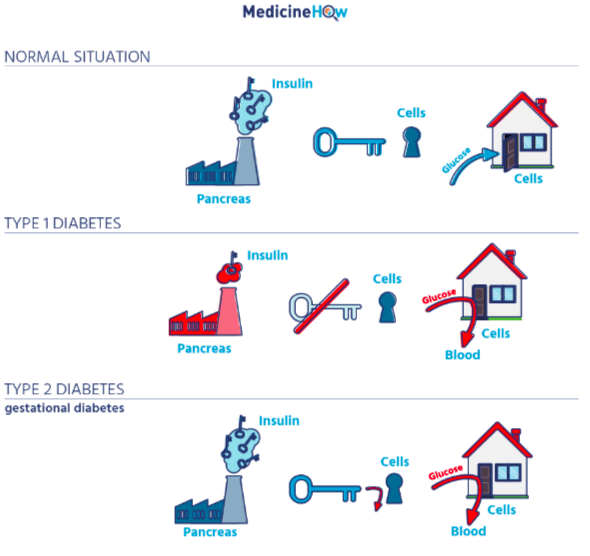
Let’s differentiate between Type 1 versus Type 2 diabetes using an analogy to help picture what is going on.
Think about how we get into a house - a factory produces keys, these keys go in the lock of the door, which allows the door to open, and then we can go inside. As you can see in the image below, what normally happens inside our body when we eat food is our pancreas (the factory) releases insulin (the key) into our blood. Insulin attaches to its receptor on the cell (the lock of a door). Insulin unlocks the receptor, which allows sugar (people) to enter the cell (the house).
It is important to understand that sugar is easily absorbed from our gut into the blood stream, but insulin and its receptor are required to get the sugar from the blood stream into our cells (things like muscles, nerves etc).
In type 1 diabetes, our pancreas is unable to make insulin because the cells that create it have been destroyed by the body’s immune system. This means there is no way to reduce our blood sugar levels after eating a meal, as there is no insulin to attach to the cell to let the sugar in. In other words, the factory does not produce the keys, meaning there are no keys to unlock the door, meaning no sugar can get into the house. This is why people who are diagnosed with type 1 diabetes require insulin injections.
Conversely, in type 2 diabetes, our pancreas often has no issues in creating and releasing insulin after we eat. The problem is the insulin becomes less effective at letting sugar into the cell - the key does not work as well in opening the locked doors. It is as if the door lock has become a bit ‘rusty’. This means sugar accumulates in the blood stream, and results in high blood sugar levels. Blood sugar levels remain high for a longer time after we eat (remember a smaller number of doors open to let sugar into the house, as some of the keys aren’t working). This is what we call ‘insulin resistance’ which is characteristic of type 2 diabetes.
Why is this a problem? Isn’t sugar essential for life? At the right level, that is true. However, when sugar levels are too high in the blood stream, sugar has a toxic effect on your body, and causes damage to a range of cells, especially those lining your blood vessels.
Now that we have established the difference, let's dig a little deeper into type 2 diabetes. For readers, it should be noted that this blog series focuses solely on type 2 diabetes from here on in and that we will cover Type 1 diabetes in a later series.
Causes of Type 2 diabetes
There are several factors which can influence your susceptibility to type 2 diabetes. Below is a list of some examples:
- Lack of physical activity
- Family history of type 2 diabetes
- Being overweight or obese
- Carrying excess weight around the waist
- Poor diet
Symptoms and health complications
Unfortunately, type 2 diabetes cannot be cured. However, the condition can be managed through lifestyle changes and, if needed, medication.
Some common symptoms of type 2 diabetes may be increased thirst, increased urination, lethargy and fatigue, increased hunger, and having cuts or wounds that heal slowly.
In the long term, because of the toxic effect of high sugar levels, type 2 diabetes can increase risk of developing other serious health complications such as kidney disease and stroke, and people with diabetes are 2-4 times more likely to develop heart disease. It can also predispose other nerve, foot, and eye problems. More than 4400 amputations occur due to diabetes each year, and diabetes is also the leading cause of preventable blindness in Australia.
The link between sugar intake and type 2 diabetes
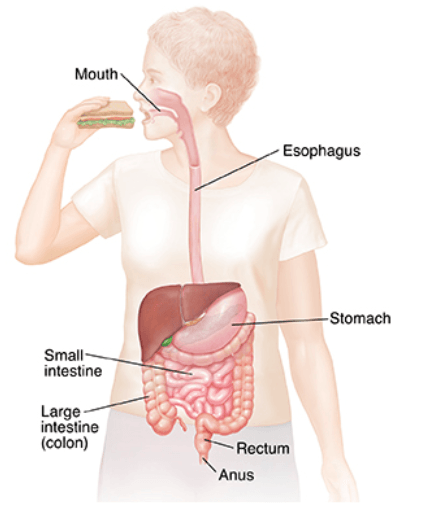
When we eat sugar, it goes down our esophagus, into our stomach, and passes into our small intestine where it is absorbed into the bloodstream. As sugar crosses into the bloodstream, blood sugar levels begin to rise, which sets off a cascade of reactions ultimately leading to the release of insulin to reduce the blood sugar levels back to normal.
Carbohydrate containing foods
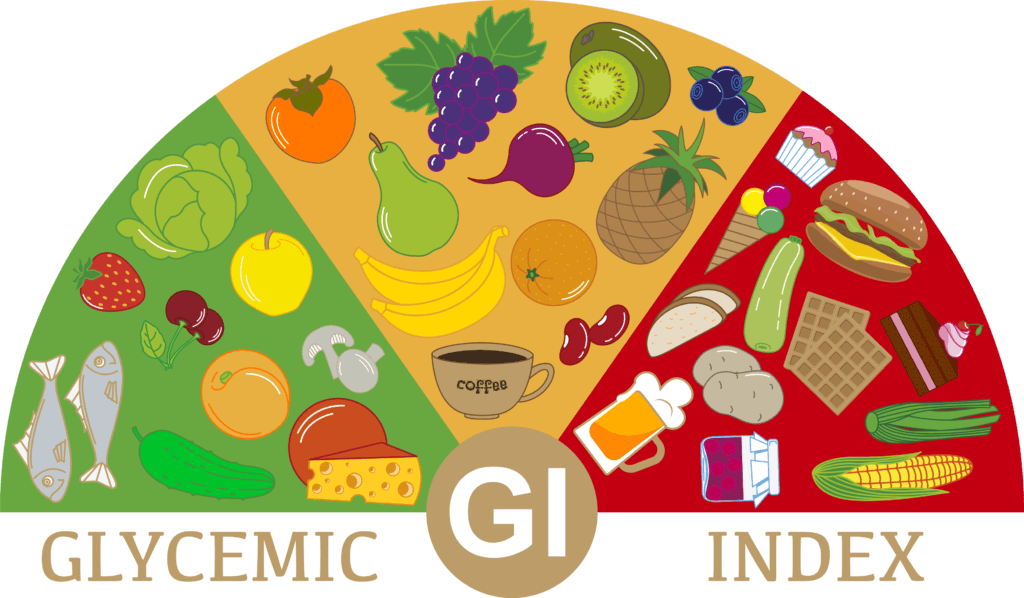
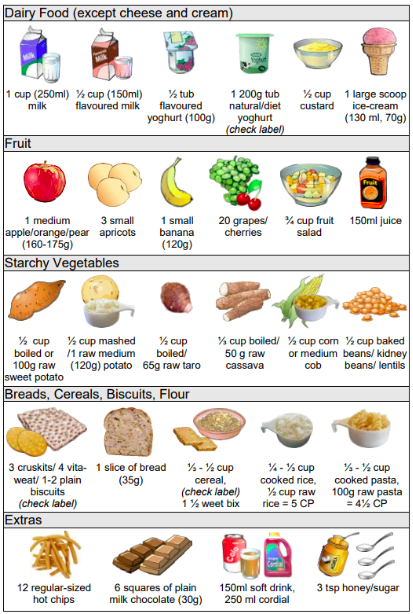
Out of the 5 food groups; fruits, dairy, and grains are the ones that commonly contain carbohydrates, meaning they will influence our blood sugar levels. Most vegetables are packed of vitamins and minerals and have negligible amounts of carbohydrates, and most meat is full of protein- again, only having small amounts of carbohydrates. As a general rule of thumb, anything that is sugary or starchy contains high levels of carbohydrate!
It is important to note, that just because a certain food contains carbohydrates does not mean it is bad, nor does it mean you should cut it out of your diet (yes, even if you have type 2 diabetes!). It should prompt you to ask: Is it high quality? How much is too much?

Portion control
As a rule of thumb, 1 serve of carbohydrates is about the size of your fist. For example, 1 piece of fruit, 1 slice of bread, 1 cup of milk, ½ cup cooked pasta or 1 scoop of ice-cream. With type 2 diabetes, we must ensure you are eating a consistent amount of carbohydrates regularly throughout the day.
Picture what would happen to your blood sugar levels if you skipped breakfast, had no morning tea, then had a huuuuuuge serve of pasta carbonara for lunch, then had a scone with cream and jam for afternoon tea, then steak and broccoli for dinner. Your blood sugar levels would drop below the normal range during the morning, then at lunch time and into the afternoon they would spike waaay above the normal range, then would drop significantly again in the evening (remember meat and vegetables have negligible amounts of carbohydrates). This stark variability will contribute to worsening insulin resistance, further perpetuating the progression of diabetes.
Now picture what would happen to your blood sugar levels if you had cereal for breakfast, a piece of fruit at morning tea, a regular sized lunch, a few biscuits and tea in the afternoon, and steak with broccoli and pasta for dinner. What do you think the biggest difference would be? Yes - that’s right! In this second example, our sugar levels would be much more consistent, and spend much more time within the healthy range. This ultimately means we are doing less damage to our vessels, and slowing the progression of this condition.
So, if there is only one thing you take away from this blog post, it would be this: Ensure consistent carbohydrate distribution throughout the day. Perhaps for you this may look like 2-3 serves of carbohydrates at your main meals, and 1-2 serves of carbohydrates at your mid-meals. Remember, this will vary from person to person, so it is recommended to get in touch with a dietitian to personalise this recommendation to your lifestyle!
Example – 1 day of eating:
Breakfast: Yoghurt + granola + banana
Morning tea: Muesli bar
Lunch: Ham + salad sandwich
Afternoon tea: Cheese + crackers
Dinner: Steak + chips + salad
Want to know more?
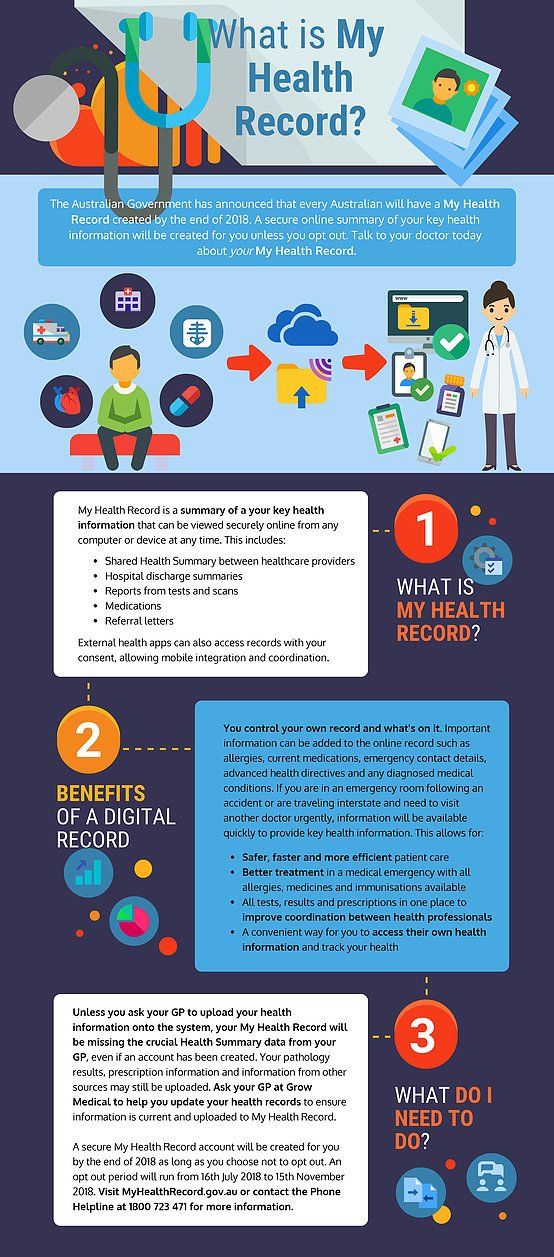
Great news - there are lots of avenues within Growlife to access more information.
- Stay tuned for part 2 of this blog series!
- Make sure you follow us on social media to keep an eye out for when the next diabetes group sessions will be. These will be run by our dietitian Jessica Cartwright.
- If this blog has got you thinking about blood sugar levels and what yours are doing - book an appointment with one of our GPs to find out. Follow this link.
- Finally, please keep in mind the contents of this blog form general information and recommendations only. If you are wanting advice tailored to your lifestyle, book a one-on-one appointment with our dietitian here.