Guide to Gestational Diabetes
Over the last 20 years in Australia, the number of people diagnosed with gestational diabetes has tripled. Through this blog, we aim to provide you with a general guide to Gestational diabetes, risk factors, symptoms, treatment and ongoing management. Should you have any concerns or further questions about your own health, we encourage you to please speak with your doctor or nurse.
Gestational diabetes is a condition where women develop high blood sugar while pregnant. Gestational diabetes generally lasts only for the duration of the pregnancy but is associated with an increased risk of Type 2 diabetes diagnosis later in life. Between 12% and 14% of pregnant women develop the condition, usually around halfway through their pregnancy.
Gestational Diabetes is caused by hormones produced by the placenta during pregnancy. These hormones help the baby to grow and develop, but also block the women’s insulin action - this is called insulin resistance. Therefore, the body requires 2 to 3 times the normal insulin levels during pregnancy. If your body is not able to cope with this extra demand, gestational diabetes may develop.
Many women living with this condition do not experience symptoms and are only diagnosed during routine testing. In about 30% of cases, women with Gestational diabetes will give birth to a larger-than-average baby. This leads to an increased likelihood of labour intervention, such as a caesarean birth. It does not mean the baby will be born with diabetes. In fact, babies of mothers with gestational diabetes have a higher likelihood of low blood sugar in the newborn period.
At their 26 to 28-week routine check-up, all women should be screened for gestational diabetes. While most women diagnosed with the condition will have a healthy pregnancy, regular delivery and a healthy baby, it is still important to be tested because untreated gestational diabetes can have serious implications for your baby, and resuls in a 50% increased risk of developing Type 2 diabetes later in life.
For more information contact a Diabetes Consultant at Growlife Medical .
Ten Gestational Diabetes Risk Factors
- are aged 40 years or older.
- have type 2 diabetes in your family history.
- have a first-degree relative (such as mother or sister) who has had gestational diabetes.
- come from an Aboriginal, Torres Strait Islander or some Asian backgrounds.
- have experienced gestational diabetes in a previous pregnancy.
- have experienced polycystic ovary syndrome.
- have previously given birth to a large baby (above 4.5kg).
- are taking some kinds of steroid or anti-psychotic medications.
- are higher than the recommended healthy weight range.
- have put on weight too quickly in the first half of your pregnancy.
Gestational Diabetes Symptoms
- higher than normal thirst levels.
- a dry mouth.
- excessive urination.
- recurring yeast infections (thrush).
- tiredness and lethargy.
- blurred vision.
Gestational Diabetes Treatment
- preparing and following a special meal plan.
- undergoing regular, scheduled physical activity.
- daily blood glucose testing and monitoring.
- if necessary, medication such as metformin or insulin injections.
Managing Gestational Diabetes
Managing Gestational diabetes should involve regular blood glucose testing, following a healthy diet and keeping on top of your doctor’s recommended exercise regime. Exercise is especially important, as it will help with other common pregnancy issues such as back pain, swelling, constipation and muscle cramping as well as managing your blood sugar levels.
Make sure to exercise only as much as your doctor recommends. Typically, you will be expected to engage in moderate physical activity for about 30 minutes a day. Depending on your fitness level, this may range from a long walk, to swimming, to cycling. Strenuous everyday activities such as cleaning and gardening may also count towards your exercise goal.
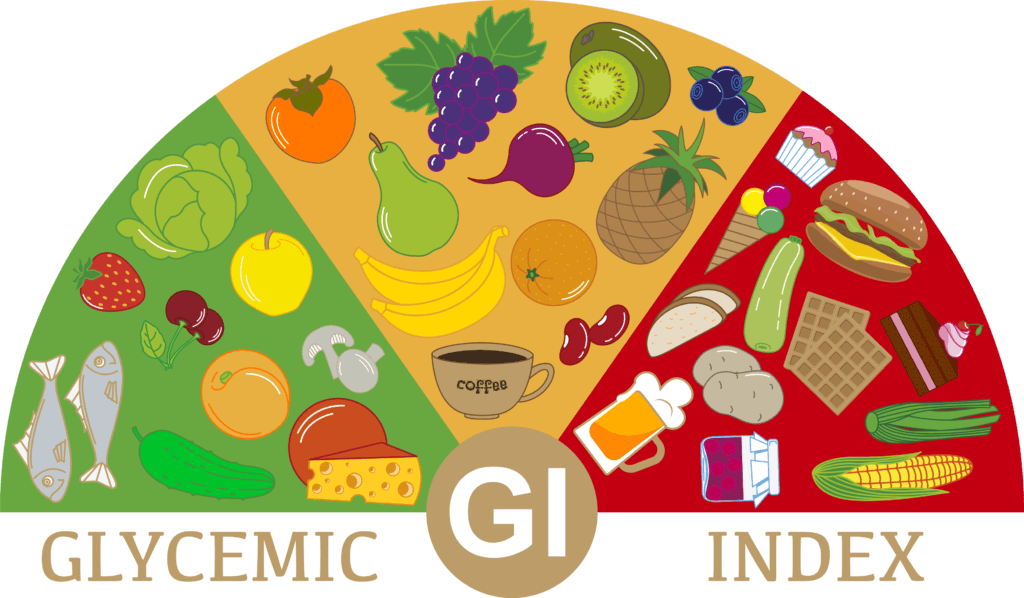
You should also follow a healthy diet during your pregnancy. This will help to ensure the general health of yourself and your baby, as well as improving your blood sugar levels. Follow your doctor or dietitian recommendations to make sure you are getting the right vitamins and minerals to support you through your pregnancy. In most cases, you should be following a diet that focuses on:
- fruit
- vegetables
- whole grains
- lean protein
- low calorie, high fibre foods
Typically, you should also avoid foods such as:
- refined carbohydrates
- sugary sweets and drinks
- high-fat, fried foods
Your GP, dietitian or diabetes specialist will help you create a simple, tasty meal plan and exercise regime to follow through the duration of your pregnancy. This should ensure your blood sugar levels remain normal. If not, it’s important to discuss this with your doctor, as you may need to start medication.
As with any pregnancy-related health condition, please be assured that health professionals, including your GP, midwife or nurse, dietitian or diabetes specialist (add booking link) will know what steps to take to treat your condition. It’s also important to talk to your family about your Gestational diabetes so they know what you are going through, and how to help you through your treatment plan.
If left untreated, gestational diabetes can have serious implications, and can result in a 50% increased risk of developing Type 2 diabetes later in life. As always, if you have any concerns, please ensure you speak with your doctor or nurse.
Gestational Diabetes Testing
Diabetes Consultation
Growlife Medical values providing community based Diabetes advice.
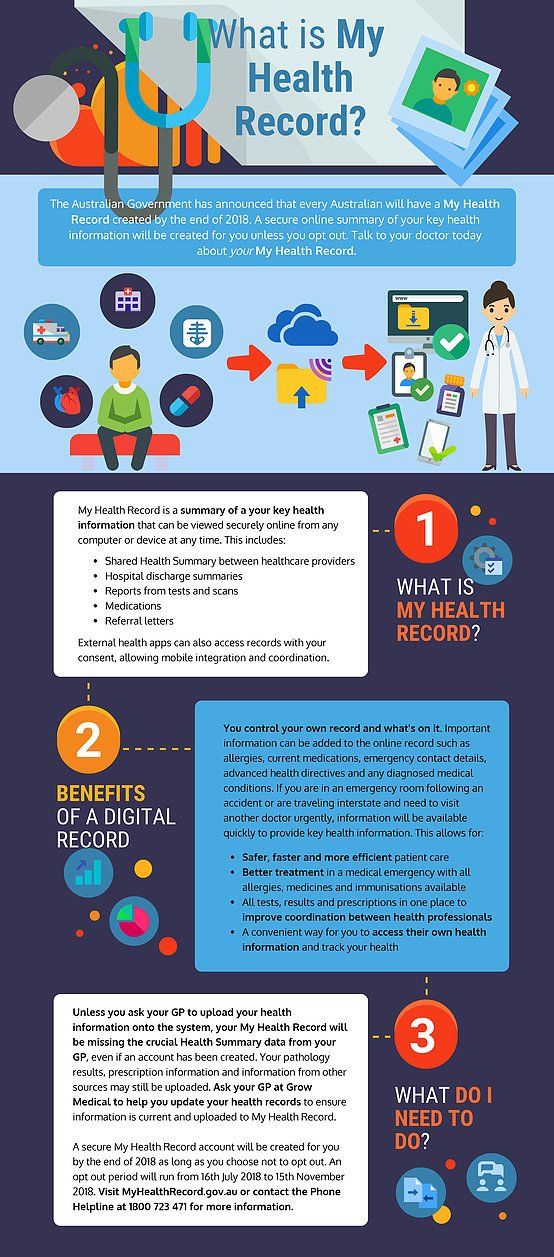
We are also Brisbane's leader in Telehealth Consults , Growlife Medical now provides easy and secure Telehealth Consults with your doctor. You can easily book online or over the phone , for a video or phone consult with your GP. All Growlife Medical Doctors in all or our general practice locations are available for Telehealth consults .
References:
https://www.diabetesaustralia.com.au/about-diabetes/gestational-diabetes/
https://www.sciencedirect.com/science/article/abs/pii/S0266613822000146

Dr Aaron Chambers
BSc, MBBS(Hons), FRACGP, Dip Child Health