Dietary Management of Diabetes

Dietary management of Diabetes, nutrition and physical exercise, both have important roles to play for people who are living with diabetes. When combined with exercise, a healthy diet plan can help to keep your blood glucose levels within the range set by your health care professional. This will give you a better quality of life and reduce the need for diabetic medications or insulin.
What you eat and when you eat are critical factors to maintaining blood glucose levels. This usually means making changes to your diet by cutting out fatty and sugary foods and carefully monitoring your calorie intake. This doesn’t sound like much fun, but diets for diabetes don’t have to be boring.
With careful management, you can create a healthy diet plan which is both nutritious and tasty. And contrary to popular belief you don’t have to completely cut out sugar or alcohol. You just have to cut down on your intake by eating smaller portions or enjoying them less often. So don’t worry, you can still have the odd treat, now and then.
The health benefits of dietary management for diabetes include:
- Helps to keep blood glucose level, blood pressure and cholesterol within the range set by your healthcare professional.
- Helps you reduce weight or maintain a healthy weight.
- Can delay or prevent the onset of complications caused by diabetes.
- Give you more energy, making you feel good for longer.
Increasing your exercise and changing your dietary habits may seem challenging at first. But humans are creatures of habit, once you get used to the new routine you may find it hard to give up. And the health benefits far outweigh any challenge you experience.
For more information contact a Diabetes Consultant at Growlife Medical.

Difference between Type 1 and 2 Diabetes
There are two types of diabetes, Type 1 and Type 2. Both are chronic conditions which affect the way your body regulates glucose or blood sugar. Glucose is the fuel your body needs to feed cells. For glucose to enter cells, insulin is produced in the pancreas, circulates in the blood stream, and acts like a key to allow glucose into cells. If a problem occurs, glucose is unable to enter the cells to provide nutrition, and builds up in the blood stream to a level where it becomes toxic.
So what is the difference between Type 1 and Type 2 Diabetes?
With Type 1 diabetes the pancreas stops producing insulin. The immune system mistakes the insulin-producing beta-cells in the pancreas as foreign invaders and destroys them. Once the cells are destroyed the pancreas is unable to produce insulin. The insulin "key" is lost, so glucose cannot enter cells, and it accumulates in the blood stream to dangerous levels. It is not certain why the immune system suddenly starts attacking healthy beta-cells in the pancreas. Some think it may be down to a virus, others say it may be genetic or the result of environmental factors.
People with Type 2 diabetes have developed insulin resistance. The pancreas still produces insulin but the body is unable to use it effectively. Using the key analogy above, it is as if the lock that allows glucose into the cells has become rusty, and so it is difficulty for glucose to enter cells. This causes the pancreas to produce more insulin to compensate, so insulin levels are high, but the glucose cannot enter cells efficiently. After many years of this process, blood glucose builds to unmanageable levels.
The reason why some people develop insulin resistance is not fully understood. A good way to understand it is that high carbohydrate consumption and excess weight, particularly around the waist, plays an important role by causing the pancreas to work on overdrive for many years. Eventually the body's cells stop responding normally to insulin, and the pancreas "burns out". Other lifestyle factors such as smoking and heavy alcohol consumption can also contribute to insulin resistance.
Type 1 Diabetes Diet
Because people with Type 1 diabetes don’t produce insulin, blood sugar levels can rise very quickly causing damage to the kidneys, eyes, and heart. Especially in those with undiagnosed type 1 diabetes, dangerous diabetic ketoacidosis can develop. People with Type 1 diabetes, therefore, need to be careful when eating foods which contain high levels of sugar such as soft drinks, white bread and pasta. Anyone with the symptoms of new onset Type 1 diabetes (increased thirst, increased urination, weight loss and fatigue) should attend their GP for a finger prick glucose test.
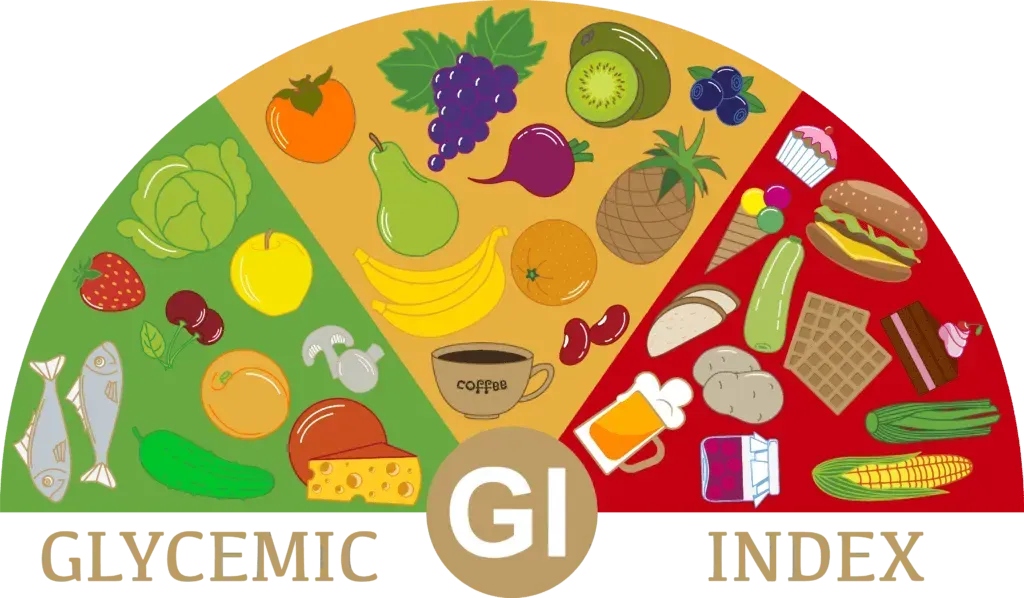
Foods typically recommended for Type 1 diabetes have a low glycemic index. The glycemic index is a measure of how quickly a food impacts blood sugar levels. Foods with a low glycemic index raise blood sugar slowly, while those with a high glycemic index raise blood sugar quickly. It is also recommended that people with Type 1 diabetes have a good understanding of calculating carbohydrate in a meal to help decide on an appropriate dose of insulin.
The timing of meals is also critical for people with Type 1 diabetes. People with Type 1 diabetes usually have to take insulin just before they eat. This ensures the body has enough insulin to absorb the glucose generated. Eating late or skipping a meal may increase a person's risk of developing low blood sugar (hypoglycemia).
The Mediterranean diet is often recommended for people suffering from Type 1 diabetes. This diet typically contains lots of fresh fish, vegetables, fruit and plant fats such as olive oil and nuts. Suggested foods to eat include whole wheat, brown rice, quinoa, oatmeal, fruit, vegetables, beans and pulses, lentils.
Unfortunately, there are a large number of foods which should be avoided by people suffering from Type 1 diabetes including:
- Soft drink (both diet and regular)
- Foods which contain simple carbohydrates. (including; processed/refined sugar, white bread, chips, cookies and some pasta)
- Foods which contain trans fats (including; high-fat animal products, and anything with the word hydrogenated on the label)
Type 2 Diabetes Diet
People suffering from Type 2 diabetes continue to produce insulin, so a dramatic onset of symptoms is uncommon. This is a problem, as many people have Type 2 diabetes but do not know, due to the lack of symptoms. Often people don’t know they have Type 2 diabetes until other complications develop such as cardiovascular disease, kidney and nerve damage.
The good news is that blood sugar levels for Type 2 diabetes can be managed well using a healthy diet. Vegetarian diets are sometimes recommended for Type 2 diabetes. But if you can’t imagine giving up meat the Mediterranean, Paleo and Keto (see below) diets are popular options because they include limited amounts of meat, fish and dairy.
Whichever diet plan you choose it should contain a mix of fats, proteins and carbohydrates. Any carbohydrates consumed should come primarily from vegetables, while fats and proteins should come from plant-based sources. The diet should consist of complex carbohydrates which are low glycemic foods and provide plenty of other nutrients such as vitamins, fibre and some proteins and fats. These all help to regulate blood sugar levels naturally.
Your diet should consist of foods with a low glycemic index and high in protein. This means a diet rich in fruit, vegetables, beans, lentils and oatmeal. You should avoid foods containing simple carbohydrates and processed foods which contain high levels of sugar or simple carbohydrate such as pasta, flour, white bread, white rice, biscuits, pastries and soft drinks (diet and regular).
Gestational Diabetes Diet
Gestational diabetes develops during pregnancy and is not a chronic condition unlike other forms of diabetes. It does mean you have a higher chance of developing Type 2 diabetes later in life. The condition is usually diagnosed in the last 12 weeks of pregnancy through the routine Glucose Tolerance Test at 26-28 weeks, and resolves after birth. If the condition continues after birth it’s usually because the patient had diabetes before falling pregnant. It is essential that an expecting mum closely adheres to a gestational diabetes diet.
Gestational diabetes is caused by hormonal changes in the body during pregnancy. This makes it more difficult for cells to use insulin properly, effectively creating a condition similar to type 2 diabetes. This means that mangement with exercise and a healthy diet is the mainstay of treatment, although due to the effect of high blood sugar on pregnancy and a growing baby, insulin is often required to keep blood glucose at an acceptable level.
Not all pregnant women will develop gestational diabetes, it affects around 16 in 100 pregnancies. Women who are overweight or clinically obese are much more likely to develop the condition. Your healthcare professional will routinely test for the condition at around twelve weeks prior to your due date, but if you feel you are in a high-risk group take advice as soon as possible.
Your diet should consist of foods which are high in complex carbohydrates including:
- Whole grain brown rice
- Buckwheat
- Whole oats
- Fruit
- Vegetables
- Pulses and lentils
- Dairy (unsweetened)
You should avoid eating foods high in sugar and simple carbohydrates including processed foods and sugary drinks such as:
- Soft drinks (both diet and regular)
- Fruit juices high in sugar
- Processed foods
- Foods high in sugar
- White bread
If you need to snack during pregnancy you should avoid biscuits, chips and chocolate. Try and stick to healthy alternatives such as unflavoured greek yoghurt (Jalna brand is a good choice), fruit, unsalted nuts and vegetables.
Keto Diet for Diabetes
Over recent years, the Ketogenic diet, or Keto diet for Diabetes, has become popular for people suffering from Type 2 diabetes. The diet is high in fat and low in carbs, which changes the way your body stores and uses energy. This eases the symptoms of diabetes by reducing demand on the pancreas for insulin release, and lowering blood glucose levels.
Several studies have shown that the Keto diet encourages the body to use fat for energy instead of glucose or carbohydrates. Participants in the studies saw improvements in glycemic control and reduced dependency for insulin.
A Keto diet doesn’t mean you can go out and load up on saturated fats though. The diet is made up of healthy monounsaturated and polyunsaturated fats, the kind which is found in vegetables and dairy products.
You should look for foods which contain high levels of protein, monounsaturated and polyunsaturated fats including:
- Eggs
- Oily fish (salmon, tuna, sardines, anchovies, mackerel)
- Avocado
- Olives
- Lean meat
- Natural cheeses
- Unsweetened yoghurt
- Nuts and berries
- Sesame seeds
You should avoid foods which contain high levels of saturated fats or sugar including:
- Low-fat dairy products (these are often sweetened)
- Grains such as rice, pasta and oatmeal
- Any food with added sugar or sweeteners
- Soft drinks (both diet and regular)
- Most fruits except lemons, limes, tomatoes and berries
- Starchy vegetables
- Any product containing trans fats, such as margarine, and many take away or deep fried foods
Potential warnings
Changing the body’s primary source of energy from carbohydrate to fat and protein is potentially dangerous for those requiring insulin to manage their diabetes. A ketogenic diet should never be commenced in those using insulin or oral medication for diabetes without medical supervision. Risks include severe low blood sugar (hypoglycaemia) and diabetic ketoacidosis.
You are therefore advised to consult a healthcare professional before trying the Keto diet. While on the diet, you should also monitor your blood sugar levels throughout the day to make sure they remain within target levels. A home testing kit is available. If you experience symptoms of DKA which include a dry mouth, frequent urination and nausea, you should contact a doctor immediately.
Other Articles On Coronavirus
Keep Up With The Latest Coronavirus in Brisbane News
Like us on Facebook to keep up to date on the Coronavirus in Brisbane.

Dr Aaron Chambers
General Practitioner
BSc, MBBS(Hons), FRACGP, Dip Child Health
Experienced author Dr Aaron Chambers has worked in General Practice since 2006. He is passionate and an authority on family practice, paediatrics and obstetric care. After completing his medical degree with honours at the University of Queensland, Dr Chambers served as an RAAF Doctor, conducting humanitarian missions and evacuating wounded servicemen from the Middle East. Dr Chambers now works alongside the combined medical experience of 20+ Doctors at Oxley, Sherwood and Highgate Hill Growlife Medical Clinics.